Understanding the Obesity Crisis and Current Treatment Limitations
The Growing Global Burden of Obesity
Obesity has become a global epidemic, affecting over 40% of the United States population and 13% of the global population. This dramatic rise in obesity rates has profound implications for public health systems worldwide, increasing the burden of obesity-related diseases and mortality. Obesity significantly increases the risk for developing multiple serious health conditions, including type 2 diabetes, cardiovascular disease, certain cancers, and metabolic syndrome. The economic burden extends beyond individual health consequences, straining healthcare systems and reducing workforce productivity globally.[1]
Limitations of Existing Weight Loss Medications
Current obesity medications, including glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Ozempic) and liraglutide, offer impressive weight loss results but come with substantial drawbacks. These medications typically require injections, which reduces patient compliance and convenience. More significantly, existing weight loss drugs frequently trigger adverse side effects including nausea, constipation, gastrointestinal distress, and significant loss of lean muscle mass alongside fat loss. The muscle loss is particularly problematic because lean body mass is essential for maintaining metabolic health and functional capacity, especially in aging populations.[2]
Most current weight loss approaches target either appetite suppression or absorption reduction—mechanisms that work by fundamentally altering eating behavior and food intake patterns. This approach can trigger adaptive metabolic responses, as the body resists calorie restriction through metabolic adaptation and increased hunger signals. Additionally, psychological challenges associated with appetite suppression and restricted eating remain significant barriers to long-term medication adherence and sustained weight loss.[3]
BMR Calculator | Basal Metabolic Rate
![]()
Metabolic Science: How Mitochondria Control Energy and Body Weight
Mitochondria: The Powerhouses of Cellular Energy
Mitochondria are specialized cellular organelles responsible for converting nutrients from food into adenosine triphosphate (ATP), the universal energy currency that powers all cellular functions. Understanding mitochondrial function is essential for understanding obesity because mitochondrial efficiency directly determines how effectively the body extracts and utilizes energy from food. Scientists have long recognized that cellular energy use shapes body weight, disease risk, and long-term health outcomes. Any intervention that alters mitochondrial activity fundamentally changes how the body processes food energy—either converting it into usable ATP or releasing it as heat.[1][4]
The Oxidative Phosphorylation Process
Mitochondria convert nutrients into ATP through a complex biochemical process called oxidative phosphorylation, which involves a series of protein complexes embedded in the inner mitochondrial membrane collectively known as the electron transport chain (ETC). As electrons move through these protein complexes, protons are pumped across the inner mitochondrial membrane, creating an electrochemical gradient. This proton gradient drives the synthesis of ATP by the enzyme ATP synthase, which acts like a molecular turbine generating chemical energy from the potential energy stored in the proton gradient.[1][4]
The efficiency of this process determines metabolic rate. When this system operates at maximum efficiency, the body extracts maximum energy from food and stores excess energy as fat. However, if this system could be made slightly less efficient, the body would need to oxidize more nutrients to produce the same amount of ATP, effectively increasing calorie expenditure without changing eating behavior or activity levels.
Biohack Your Longevity at Cellular Level – Novomins Nutrition
Cellular Respiration: Steps, Process, and Stages | Osmosis
![]()
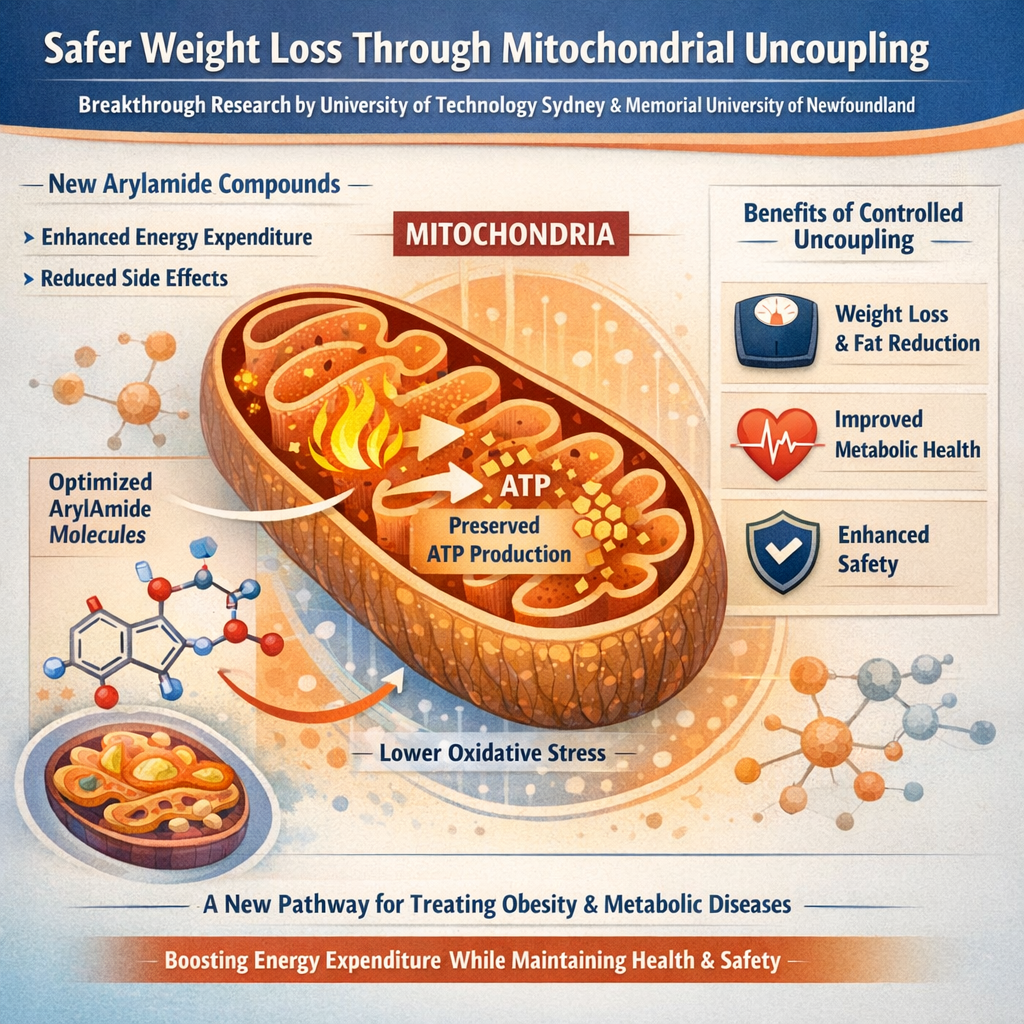
Mitochondrial Uncoupling: A New Approach to Weight Loss
What Is Mitochondrial Uncoupling?
Mitochondrial uncoupling is a process where the coupling between electron transport and ATP synthesis is disrupted, allowing protons to bypass ATP synthase and dissipate the proton gradient as heat instead of using it to generate ATP. In healthy cells, this proton gradient is tightly controlled to maximize ATP production. During uncoupling, part of the energy from food escapes as heat rather than being stored as ATP, effectively creating metabolic inefficiency.[4]
Professor Tristan Rawling from the University of Technology Sydney explains the process using a hydroelectric dam analogy: "It's been described as a bit like a hydroelectric dam. Normally, water from the dam flows through turbines to generate electricity. Uncouplers act like a leak in the dam, letting some of that energy bypass the turbines, so it is lost as heat, rather than producing useful power." Small leaks raise heat output while power generation continues uninterrupted. Large leaks drain power entirely. The safety profile depends on the size of the "leak," not whether uncoupling occurs.[1]
The Key Difference: Mild vs. Severe Uncoupling
The critical distinction in modern research is the difference between full uncoupling, which collapses energy production entirely and poses severe health risks, and mild uncoupling, which weakens efficiency without shutting down ATP synthesis. In mild uncoupling, cells continue producing essential ATP needed for vital functions while simultaneously burning additional fuel to compensate for the lost energy efficiency. This represents a fundamental shift in how metabolic drugs could work—rather than forcing extreme metabolic changes, newer research explores controlled inefficiency.[1]
![]()
The Dark History of Mitochondrial Uncoupling: Learning from Past Mistakes
2,4-Dinitrophenol (DNP): A Cautionary Tale
During World War I, munitions workers in France who handled a chemical called 2,4-Dinitrophenol (DNP) experienced unexplained weight loss, elevated body temperatures, and in some cases, death. Scientists investigating this occupational hazard discovered that DNP functions as a mitochondrial uncoupler. DNP was briefly marketed in the 1930s as one of the first weight-loss drugs and proved remarkably effective, with approximately 90% of patients taking 300 mg DNP daily losing 2-3 pounds per week without changes in food intake.[1][5]
However, the therapeutic window for DNP proved dangerously narrow. The dose required for weight loss and the lethal dose were perilously close, making overdose a serious risk. DNP caused severe toxic effects including uncontrollable hyperthermia (overheating), neuropathy, and death. Because DNP's effects are dose-dependent and individual variation in drug metabolism is significant, determining a safe dose for each patient proved impossible. The drug was subsequently banned due to these severe safety issues, and DNP became a cautionary tale in pharmaceutical development.[1]
Why Modern Research Is Different
Modern research approaches the problem fundamentally differently by focusing on controlled, mild uncoupling rather than extreme metabolic disruption. The key breakthrough is understanding that proton transport rate—not just the presence of uncoupling—determines the biological outcome. Fast proton transport shuts down ATP production entirely, creating the dangerous toxicity seen with DNP. Slower proton transport lowers metabolic efficiency while maintaining adequate energy supply, creating a safer therapeutic window.[1]
This understanding enables researchers to design molecules with unprecedented precision, tuning the strength of uncoupling to a safe and effective level.
![]()
Modern Mitochondrial Uncouplers: Scientific Innovation and Design
Arylamide Compounds: The New Generation
Recent research describes experimental arylamide compounds that act as mild mitochondrial uncouplers, with research teams focusing specifically on how fast protons move across mitochondrial membranes. The molecular structure of these compounds determines their functional properties. Arylamide molecules vary based on aromatic substitution patterns, and specific patterns allow strong dimer formation and rapid proton movement, while other patterns weaken dimer stability and slow proton transport.[1]
This molecular-level understanding enables researchers to engineer molecules with precisely calibrated uncoupling strength. By reducing dimer stability, researchers can slow proton transport, producing mild uncoupling rather than full collapse of energy gradients. This represents genuine innovation in drug design—moving from trial-and-error approaches to rational molecular engineering.
Membrane Studies and Transport Rate Control
Experiments using simplified membrane systems isolate proton movement from other cellular processes, revealing that proton transport speed governs biological outcome. These studies demonstrate a surprising principle: some molecules enter membranes quickly yet move protons slowly, while other molecules accumulate more slowly but later reach high transport speeds. Transport rate, not dose alone, defines safety, establishing a clear design principle where control over proton transport rate allows separation of benefit from danger.[1]
This breakthrough means that researchers can now design safer uncouplers by fine-tuning molecular properties rather than simply adjusting dose—a fundamentally more robust approach to safety.
Pharmaceutical development laboratory | Tecnalia
Drug Discovery and Development Process | PPD
![]()
Health Benefits Beyond Weight Loss
Enhanced Calorie Burning Without Behavioral Change
Mild uncoupling raises cellular respiration while preserving ATP levels, allowing cells to continue essential work while burning extra fuel. This metabolic approach offers a fundamentally different pathway compared to appetite suppressants. Unlike GLP-1 medications that work by reducing food intake and can cause psychological challenges related to appetite restriction, mitochondrial uncoupling does not suppress appetite or trigger compensatory eating behavior. The body's mesolimbic reward center remains unaffected, avoiding the psychological burden associated with dietary restriction.[1][3]
Studies show that when animals are treated with mitochondrial uncouplers like BAM15, they consume the same amount of food as controls but achieve significant fat loss, with no changes in food intake, lean body mass, or body temperature. This separation of fat loss from appetite suppression and behavioral change represents a genuinely novel approach to weight management.[5]
Reduction in Oxidative Stress and Metabolic Health
An important advantage of mild mitochondrial uncoupling is that it reduces oxidative stress in cells, which could support metabolic health and provide anti-aging effects. Paradoxically, while increasing overall energy expenditure might seem to increase oxidative stress (since oxidative phosphorylation is the source of reactive oxygen species), mild uncoupling actually reduces reactive oxygen species production.[1]
This occurs because mild uncoupling lowers the proton gradient, which reduces the driving force for electrons backing up in the electron transport chain—the primary source of superoxide production. The result is decreased oxidative damage, improved cellular antioxidant status (increased glutathione), and decreased inflammatory markers. These antioxidant benefits may protect against age-related diseases and neurodegenerative conditions such as dementia and Alzheimer's disease.[6][1]
Improved Metabolic Health Markers
Recent clinical trials demonstrate that newer mitochondrial uncouplers improve multiple metabolic health markers beyond simple weight loss. Studies show improvements in insulin sensitivity across multiple tissue types, reduced liver fat content, decreased hepatic steatosis, and improved lipid profiles. A Phase 2a clinical trial with HU6, a controlled-release mitochondrial protonophore, demonstrated a mean reduction in liver fat content of 33% in patients with nonalcoholic fatty liver disease without serious adverse events. The drug also induced body fat loss without statistically significant loss of lean body mass, representing a major advantage over traditional weight loss medications.[6]
![]()
Emerging Clinical Evidence and Drug Development
BAM15: Preclinical Success in Animal Models
Research with BAM15, a mitochondrial uncoupler candidate, demonstrates powerful anti-obesity and metabolic benefits in preclinical models. BAM15 is orally bioavailable, increases nutrient oxidation dose-dependently, and decreases body fat mass in mice fed a Western diet without altering food intake or decreasing lean body mass. Key findings include a 54% increase in respiration rate in liver tissue from BAM15-treated mice compared to controls, while muscle showed a non-significant trend for increased respiration and adipose tissue respiration was unchanged.[5]
Metabolomic analysis of liver tissue shows that BAM15 treatment had no major destabilization of the overall metabolic profile, with the strongest signatures being antioxidant effects including increased glutathione, decreased bioactive oxidized lipids, and decreased pro-inflammatory lipid mediators. ATP levels remained normal in liver tissue, and there was no indication of energy stress via AMPK signaling, indicating that nutrient flux through mitochondria was sufficient to maintain normal physiology.[5]
HU6: Recent Clinical Trial Data
The HuMAIN-HFpEF randomized clinical trial tested HU6 in patients with obesity-related heart failure with preserved ejection fraction (HFpEF), a common condition where excess body fat plays a pivotal role in disease development. The trial included 66 participants with mean age 64.5 years randomized to HU6 treatment for 19 weeks (starting at 150 mg daily and potentially escalating to 450 mg daily) or placebo.[6]
Results showed that HU6 (versus placebo) significantly decreased weight (between-group difference: -2.86 kg), total fat mass (between-group difference: -2.96 kg), and percentage visceral fat. Importantly, HU6 demonstrated good safety and tolerability, with no serious adverse events reported. This represents genuine progress toward bringing mitochondrial uncoupling therapy from laboratory research to clinical practice.[6]
SANA: A Novel Approach to Energy Expenditure
Stanford researchers have identified SANA, a nitroalkene derivative of salicylate, as a first-in-class activator of creatine-dependent energy expenditure and thermogenesis. SANA functions through a different mechanism than protonophore uncouplers, enhancing mitochondrial respiration and increasing creatine-dependent energy expenditure in adipose tissue. SANA reduces liver steatosis and insulin resistance in preclinical models and demonstrates beneficial effects on body weight and glucose management within two weeks of treatment in a Phase 1A/B clinical trial.[2]
Adenosine triphosphate (ATP) | Definition, Structure ...
![]()
Policy and Regulatory Considerations for Future Development
The history of mitochondrial uncoupling clearly demonstrates that safety must be the paramount concern in drug development. Modern regulatory frameworks have learned from the DNP disaster and require rigorous preclinical toxicology testing, careful dose escalation in clinical trials, and long-term safety monitoring. Current pharmaceutical approaches emphasize tissue targeting—particularly liver-targeted formulations—to concentrate drug effects where metabolic improvement is most needed while minimizing systemic exposure and potential adverse effects.[6]
The Importance of Long-Term Data
While emerging clinical data are promising, long-term safety and efficacy data are essential before mitochondrial uncouplers can be broadly recommended for weight loss. Current Phase 2a trials represent early-stage clinical testing. Before reaching Phase 3 (definitive efficacy) or FDA approval, researchers need extended studies in larger patient populations, assessments of long-term tolerance development, evaluation of drug interactions, and monitoring for delayed adverse effects.[7]
![]()
Comparison with Other Emerging Weight Loss Approaches
GLP-1 Receptor Agonists vs. Mitochondrial Uncouplers
While GLP-1 receptor agonists like semaglutide and tirzepatide achieve significant weight loss through appetite suppression, they have important limitations including gastrointestinal side effects, potential loss of lean muscle mass, and psychological challenges associated with appetite restriction. These medications work by activating receptors throughout the body—not just in appetite centers—causing widespread metabolic effects. Mitochondrial uncouplers represent a complementary approach working through a fundamentally different mechanism, potentially offering advantages for patients who cannot tolerate GLP-1 medications or prefer a metabolism-based approach.[2][6]
Natural Approaches: Brown Adipose Tissue Activation
Researchers have identified that caffeine exposure can induce browning of white adipose tissue, increasing uncoupling protein 1 (UCP1) expression and thermogenesis in brown adipocytes. This natural activation of brown fat thermogenesis represents another potential approach to increasing energy expenditure. However, the magnitude of effect from caffeine is modest compared to pharmaceutical uncouplers, highlighting why drug development remains valuable for more severe obesity.[8]
Total Daily Energy Expenditure Calculator | by Dr Bill Sukala
![]()
Future Directions and Therapeutic Potential
Timeline for Clinical Availability
While the research framework is strong, mitochondrial uncouplers remain in early-stage development with most candidates still in preclinical or Phase 1-2 trials. Realistic timelines for FDA approval and clinical availability likely extend 5-10 years for the most promising candidates. However, accelerated development pathways and breakthrough therapy designations could potentially shorten this timeline if clinical efficacy continues to improve.[7]
Future obesity treatment may involve combination approaches pairing mitochondrial uncouplers with other therapies such as GLP-1 receptor agonists, to target multiple pathways simultaneously and achieve synergistic effects. Combining a metabolism-enhancing mitochondrial uncoupler with an appetite-suppressing GLP-1 agonist could potentially provide superior weight loss and metabolic benefits compared to either approach alone.[7]
Beyond obesity, mitochondrial uncoupling research suggests potential therapeutic applications for metabolic syndrome, fatty liver disease, type 2 diabetes, cardiovascular disease, and neurodegenerative conditions. The antioxidant effects of mild uncoupling could provide disease-modifying benefits for aging-related conditions, making mitochondrial uncouplers potentially valuable across multiple disease areas.[1][6]
![]()
What Consumers Should Know: Key Takeaways
Current Status and Availability
Mitochondrial uncouplers remain experimental compounds under active research and development. They are not currently available for clinical use or weight loss outside of clinical trials. Consumers should be cautious of any supplements or products claiming to provide "mitochondrial uncoupling" benefits—current research compounds are available only through clinical trials at research institutions.
The history of DNP provides an important reminder that weight loss drugs carry risks. Any future mitochondrial uncouplers must demonstrate clear safety margins through rigorous testing. The fact that modern research is specifically focused on mild, controlled uncoupling represents genuine progress in addressing historical safety concerns.
Mitochondrial uncouplers offer a fundamentally different approach to obesity treatment, working through metabolic enhancement rather than appetite suppression. For patients who experience intolerable side effects from existing medications or who prefer an alternative mechanism, these drugs could eventually provide valuable options. The research demonstrates that scientific innovation can address the limitations of first-generation weight loss drugs.
![]()
Conclusion: A Paradigm Shift in Weight Loss Pharmacotherapy
The research on mitochondrial uncoupling represents a significant paradigm shift in how scientists approach obesity treatment. Rather than forcing weight loss through appetite suppression—an approach that triggers compensatory metabolic responses and psychological challenges—mitochondrial uncouplers offer to increase baseline energy expenditure through controlled metabolic enhancement. This fundamental difference in mechanism could provide advantages for many patients struggling with existing weight loss medications.[1]
The history of mitochondrial uncoupling, from the toxic effects of DNP in the 1930s through modern controlled approaches, demonstrates how scientific understanding can transform dangerous concepts into therapeutic opportunities. By precisely tuning molecular structure to control proton transport rate, researchers have moved beyond the dangerous all-or-nothing uncoupling of historical compounds to develop safer, more selective interventions. Emerging clinical data from Phase 2a trials demonstrate that modern mitochondrial uncouplers can achieve meaningful fat loss, improve metabolic health markers, and show good safety and tolerability.[6][1]
While still in early stages of development, mitochondrial uncouplers represent one of the most promising new approaches to obesity treatment on the horizon. Combined with continued research on other novel mechanisms, advancing GLP-1 receptor agonists, and improvements in lifestyle interventions, these drugs could offer patients multiple therapeutic options tailored to individual needs and preferences. The journey from DNP's dangerous legacy to safe, effective mitochondrial uncouplers exemplifies how scientific progress, coupled with rigorous safety oversight, can transform metabolic medicine for the better. The future of weight loss treatment will likely involve personalized approaches selecting from multiple mechanisms—and mitochondrial uncoupling will play an important role in that future.[1]







Post your opinion
No comments yet.